Genotyping has proven most no known risk HCV infections in the EU are healthcare based
Below 3 important studies into Hepatitis C genotypes clearly show that Europeans presenting with hepatitis c infections without a known risk had the same profile of genotypes as those infected via transfusions. Importantly this was common knowledge in mainland Europe from 1995 yet such facts have never been clarified by our Department of Health.
The second genotype study in the US showed again that many genotype 1a Hepatitis C infections were also from healthcare sources rather than behaviours.
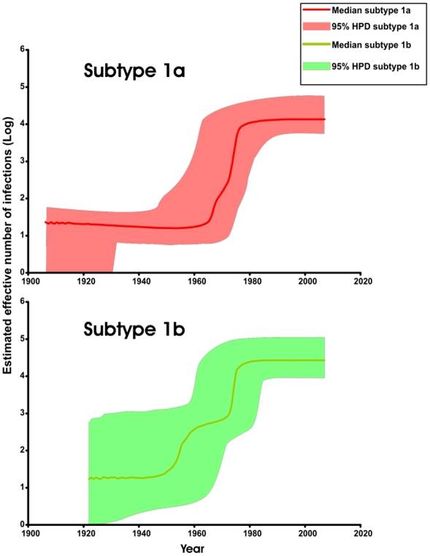
The third study shows that from 1940 to 1965 the West had its first boom of hepatitis c mainly from syringe re use and then from 1965 to 1991 from transfusions. Needless to say just as the UK has never mass tested its generation exposed to tainted blood healthcare, it has never carried out or acted on these type studies.
Relationship between Hepatitis C Virus Genotypes and Sources of Infection in Patients with Chronic Hepatitis C
Jean-Michel Pawlotsky, Laurent Tsakiris, Françoise Roudot-Thoraval, Claire Pellet, Lieven Stuyver, Jean Duval, Daniel Dhumeaux; J Infect Dis 1995; 171 (6): 1607-1610. doi: 10.1093/infdis/171.6.1607 Published: 01 June 1995
Abstract
This study examined the relationships between hepatitis C virus (HCV) genotypes and the routes of HCV transmission in 101 patients with chronic hepatitis C.
Patients who received
blood transfusions (43%) and those with chronic hepatitis C of
unknown cause (37%) had similar mean ages, age distribution, and HCV genotype distribution
(la, 19% vs. 14%; 1b, 52% vs. 54%; 3a, 10% vs, 9%; other, 19% vs. 23%).
Intravenous drug users were significantly younger and had a different genotype distribution (1a, 33%; 1b, 0; 3a, 63%; other, 5%; P < .001). Transmission of HCV 3a has been observed only over the past 20 years; other genotypes were transmitted up to 40 years ago. These results suggest that for 20 years there have been two independent ongoing hepatitis C epidemics. One affects persons who received blood transfusions or whose source of infection is unknown. These persons are older and are mainly infected by HCV 1b. The second type of infection occurs in IVDUs and infects younger persons, mainly with HCV 3a.
Looks Like Boomers Didn’t Get Hepatitis C From Youthful Drug Use After All
https://www.hepmag.com/article/looks-like-boomers-get-hepatitis-c-youthful-drug-use
April 13, 2016
A new study challenges the prevailing wisdom that high rates of hepatitis C virus (HCV) among members of the baby boom generation are a result of their youthful experimentation with drugs, unsafe tattooing and risky sex, aidsmap reports. Publishing their findings in The Lancet Infectious Diseases, researchers analyzed 45,316 sequences of genotype 1a of hep C, which is the dominant strain in North America. The scientists concluded that hep C saw its greatest infection rates between 1940 and 1965. These rates tapered at the end of this period and plateaued between 1965 and 1989. The 1990s saw falling infection rates, and starting in 2000, the rates rose modestly.
These patterns suggest that, in fact, unsafe medical procedures are the root cause of the virus’s spread among baby boomers. This generation was too young during the period of the epidemic’s vast expansion for members to have largely contracted the virus from behaviors—including injection drug use—that are more common among young adults. Furthermore, the post–World War II era saw a great upswing in the number of medical procedures. Proper safety measures, such as the introduction of disposable syringes during the 1950s, were slower to come onto the scene.
Blood transfusions were likely largely responsible for transmissions between 1965 and 1989 given that thorough screening for hep C in the blood supply did not begin until 1992.
The spread of hepatitis C virus genotype 1a in North America: a retrospective phylogenetic study.
Lancet Infect Dis. 2016 Jun;16(6):698-702. doi: 10.1016/S1473-3099(16)00124-9. Epub 2016 Mar 30
Joy JB1, McCloskey RM2, Nguyen T2, Liang RH2, Khudyakov Y3, Olmstead A4, Krajden M5, Ward JW3, Harrigan PR6, Montaner JS6, Poon AF6.
The expansion of genotype 1a before 1965 suggests that nosocomial or iatrogenic factors (blood transfusions, unsterile medical equipment and injections and blood products) rather than past sporadic behavioural risk were key contributors to the hepatitis C virus epidemic in North America. Our results might reduce stigmatisation around screening and diagnosis, potentially increasing rates of screening and treatment for hepatitis C virus.
The global spread of hepatitis C virus 1a and 1b: a phylodynamic and phylogeographic analysis.
PLoS Med. 2009 Dec;6(12):e1000198. doi: 10.1371/journal.pmed.1000198. Epub 2009 Dec 15.
Magiorkinis G1, Magiorkinis E, Paraskevis D, Ho SY, Shapiro B, Pybus OG, Allain JP, Hatzakis A.
We showed that transmission of subtypes 1a and 1b "exploded" between 1940 and 1980, with the spread of 1b preceding that of 1a by at least 16 y (95% confidence interval 15-17). Phylogeographic analysis of all available NS5B sequences suggests that HCV subtypes 1a and 1b disseminated from the developed world to the developing countries.
CONCLUSIONS:
The evolutionary rate of HCV appears faster than previously suggested. The global spread of HCV coincided with the widespread use of transfused blood and blood products and with the expansion of intravenous drug use but slowed prior to the wide implementation of anti-HCV screening. Differences in the transmission routes associated with subtypes 1a and 1b provide an explanation of the relatively earlier expansion of 1b. Our data show that the most plausible route of the HCV dispersal was from developed countries to the developing world.